GENERAL
What is glaucoma?
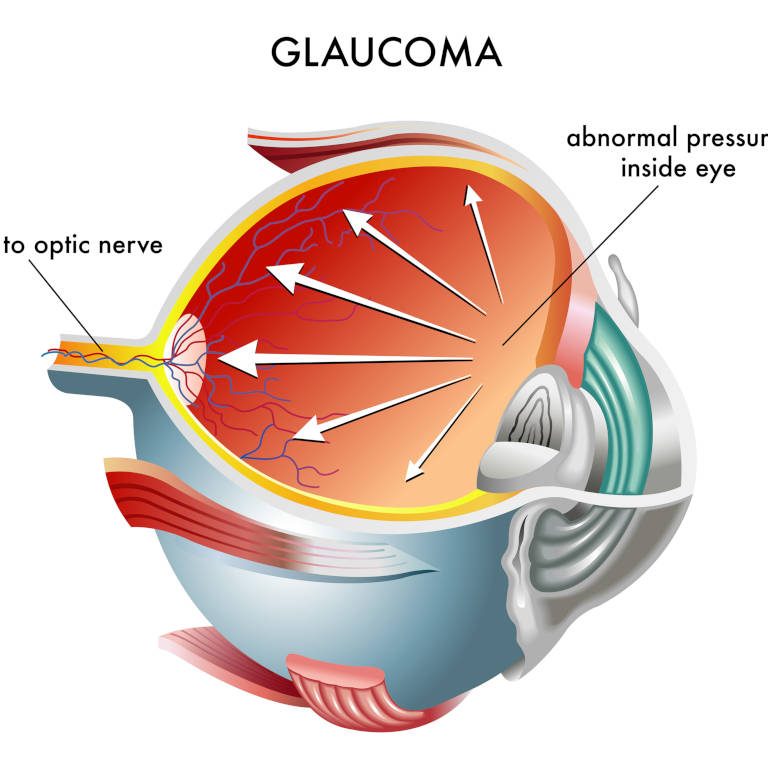
We use the term glaucoma for the disease of the eye in which the optic nerve is damaged, usually due to high intraocular pressure.
The optic nerve transmits information from the eye to the brain and as it is gradually affected, by increased pressure inside the eye, the vision gets worse.
The damage of the optic nerve causes misty and patchy vision, initially peripherally, and in the final stages it can cause loss of the central vision as well.
The damage caused to vision by glaucoma due to destruction of the optic nerve unfortunately is irreversible.
However, with timely diagnosis, careful management, rigorous follow-ups and the use of innovative treatments that Ophthalmology can now offer, progression of the damage of the optic nerve can be halted to a great extent and the vast majority of people suffering from glaucoma can maintain satisfactory levels of vision for the rest of their lives.
Prevention through regular checkups can save our vision!
How many types of glaucoma exist?
There are four main types of glaucoma:
- Primary open angle glaucoma. It is the most common type of glaucoma. It is also known as chronic open angle glaucoma and it is often called “the silent thief of our vision”, because at its initial stages it presents no warning signs, such as pain, loss of the eyesight or other indications that something is wrong. Due to the nature of this condition and the irreversible loss of visual field that it can cause while progressing, it is necessary that you check your eyes regularly to make sure that you are not developing high intraocular pressure or that your primary open angle glaucoma is stable and well managed.
- Primary angle closure glaucoma. This specific type is related to the mechanical closure of the drainage angle in the anterior chamber of the eye mainly due to anatomic variation of the eye structures. More specifically, the iris prevents the free drainage of the aqueous humor from the anterior chamber of the eye through the trabecular meshwork outside the eye. Regular checkups by an Ophthalmologist with a special test called gonioscopy can timely identify patients at risk of developing acute angle closure glaucoma and take preventative measures by performing a laser procedure called laser iridotomy.
- Secondary glaucoma. It refers to the types of glaucoma caused by third causes such as injury, intraocular inflammatory conditions, pigment dispersion, pseudo exfoliation material as well as serious cases of cataract or diabetes. The management depends on the primary cause as well as the severity of presentation and the treatment plan always take into consideration all associated factors.
- Pediatric or congenital glaucoma. It is a type of glaucoma that develops during the first years of childhood. The diagnosis of glaucoma to babies and children is almost always associated with increased intraocular pressure.
Causes
What causes glaucoma?
Glaucoma is caused by an imbalance in the production and drainage of the clear aqueous humor filling the anterior chamber of the eye (the space between the cornea and the iris). The aqueous humor is produced on a daily basis by the ciliary body inside the eye and it is drained by the trabecular meshwork outside the eye in the episcleral veins. Usually, glaucoma is the result of gradual blockage of the drainage through the trabeculum from the anterior chamber of the eye, from where aqueous humor normally exits the eye.
As the quantity of aqueous humor increases, the pressure inside the eye increases as well, affecting the optic nerve fibres and depriving it from oxygen and other nourishing factors.
As time goes by and the condition remains untreated or poorly managed, unacceptable levels of intraocular pressure cause gradual irreversible damage to the nerve and subsequent loss of visual field.
Secondary glaucoma may have as a cause other eye conditions, such as tumors, detached retina, central retinal vein or artery occlusion, eye trauma, hypermature cataract as well as other health conditions such as uncontrolled diabetes.
In pediatric or congenital glaucoma, the drainage system of the eye has not developed properly from birth so the aqueous humor builds up inside the eye leading to high intraocular pressure.
In some cases, the optic nerve shows glaucomatous damage confirmed on visual field test with corresponding defects while the patients have intraocular pressure within the normal range. This type of glaucoma is called normal tension glaucoma and the causes seem to be less clear.
On the contrary, a person may have high intraocular pressure (above 22mmHg) without having developed glaucoma. This condition is called ocular hypertension, which if not treated timely may lead after several years to the development of glaucoma.
What are the risk factors for glaucoma development?
The factors that increase the risks of glaucoma development include the following:
- Age. The risk for glaucoma increases significantly after the age of 40 and continues to increase every ten years. This is partially due to the fact that ageing may cause shrinking or narrowing of the drainage channels inside the trabecular meshwork.
- Medical problems. Conditions such as diabetes, migraines, low blood pressure, cardiovascular diseases and low cerebrospinal fluid pressure are considered risk factors for the development of chronic open angle glaucoma. Long-term high dosage steroid use, in the form of tablets or inhalers increases the possibility of development of glaucoma.
- Anatomic abnormalities. Possible abnormalities in the internal structures of the eye may obstruct the drainage system of the eye and cause glaucoma.
- Race. Chronic open angle glaucoma is three to four times more frequent in people of African origin.
- Heredity. The risk of developing glaucoma is three to four times higher if one or more first degree relatives have developed the disease.
- Way of living. The sedentary lifestyle, without regular exercise, may increase the risk for glaucoma, according to research.
Symptoms
When should I see my ophthalmologist?
Chronic glaucoma does not present any warning symptoms during its initial stages. The patient might have high intraocular pressure but not feel any pain and usually is unaware of the damage caused to his visual field. This is due to the fact that the damage is caused initially to the peripheral parts of the visual field and therefore central vision is spared until the late stages of the disease. Also, glaucoma in most cases does not affect both eyes to the same degree so the eye that is less affected usually compensates for the other one .Therefore the patient does not perceive scotomata (blind spots) in his visual field until it is too late.
On the contrary, acute glaucoma tends to be particularly painful, due to the sudden increase of intraocular pressure. Some of the symptoms are haloes around lights, eye redness, blurry vision and sometimes discomfort, severe headache, nausea and vomiting.
In pediatric (congenital) glaucoma, there is increase in the volume of the eyes , reduction of eyesight, light sensitivity, while the eyes look red and tearful.
Diagnosis
How is glaucoma diagnosed?
The evaluation of the patient suffering from glaucoma includes a complete eye examination, vision test, measurement of the pressure of the eye and pachymetry of the thickness of cornea.
It also includes gonioscopy, examination of the anterior chamber of the eye in order to verify if the drainage angle is open as well as fundoscopy to check the optic nerve.
If there is a hint of glaucoma, then there are imaging tests of the optic nerve, such as the visual field test and analysis of the retinal nerve fibre layer called disc optical coherence tomography (OCT). The latter is a new examination thanks to which there is detailed mapping of the posterior structures of the eye as well as of the optic nerve and it can detect damage at a very early stage.
If these tests show that the optic nerve and the visual field are normal and there is still high intraocular pressure then the diagnosis might be ocular hypertension, which is associated with high intraocular pressure without glaucomatous damage to the optic nerve.
The effect of ocular hypertension on the optic nerve of the patient is checked, mainly with optical coherence tomography (OCT), which can detect damage to the optic nerve before it appears on the visual field test. If there is evidence that it begins to cause even the mildest damage to the optic nerve, then measures are taken in order to reduce intraocular pressure. This can be achieved in several ways, such as prescription of special pressure lowering drops for the eye or a special laser procedure called Selective Laser Trabeculoplasty (SLT).
Therapy
How is glaucoma treated?
The damage caused to the eyesight by glaucoma is irreversible. That is why the treatment focuses on slowing down the effects of the disease on the optic nerve and therefore prevention of sight loss and visual field loss.
The earliest glaucoma is diagnosed and treated, the least damage to the optic nerve is bound to happen, ensuring satisfactory levels of eyesight for the rest of the patient’s life.
The main aim of glaucoma treatment is reduction of pressure inside the eye.
According to the mechanism and gravity of glaucoma, the reduction of intraocular pressure can be achieved in different ways, such as:
- Daily use of medication in the form of eye drops. The treatment of glaucoma often begins with the prescription of special eye drops (prostaglandin analogs, b blockers, carbonic anhydrase inhibitors, a adrenergic inhibitors), which contribute to the reduction of intraocular pressure. Tablets taken orally for the reduction of intraocular pressure are sometimes used as last resort, if the treatment with eye drops is inefficient or impossible due to local allergy.
- Selective Laser Trabeculoplasty (SLT). It is a minimally invasive method being performed as an outpatient by an eye doctor specializing in glaucoma. It uses laser beams targeted towards specific areas of the trabecular meshwork and it achieves reduction of intraocular pressure through facilitation and augmentation of drainage of the aqueous humor.
- Endocyclophotocoagulation (ECP). Another minimally invasive endoscopic method that uses laser beams in order to reduce the pressure inside the eye through the inhibition of the production of fluid by the ciliary body.
- Surgical operation (safe trabeculectomy, glaucoma drainage device placement). It is selected for the more advanced and rapidly progressive cases of glaucoma.
- Transscleral cyclophotocoagulation. It uses laser beams that are applied locally on the ciliary body in order to reduce pressure inside the eye through the inhibition of the production of aqueous humor and mainly applies to end stage glaucoma cases.
Selective Laser Trabeculoplasty (SLT) is a minimally invasive method, a laser procedure that we opt for when eye drops do not reduce the intraocular pressure enough or when they cause significant side effects or even instead of starting eye drops for early glaucoma.
Ideal candidates for this type of therapy are patients with early primary open angle glaucoma or ocular hypertension.
During the SLT procedure, a laser beam is directed to specific areas of the drainage system of the eye activating cells in that area to improve their function and drain better the aqueous humor so that the intraocular pressure goes down. The procedure itself takes only a few minutes, it is pain free and it may be performed as an outpatient by a glaucoma specialist. There is a three month wait period from the day of the surgery until the effect of the treatment to the pressure becomes evident.
Selective Laser Trabeculoplasty does not produce fibrosis so it can be repeated as many times as we need and it is totally painfree.
Endocyclophotocoagulation is a new, minimally invasive endoscopic method, which uses laser technology to reduce intraocular pressure. With this procedure we can reduce the need for eye drops for patients with moderate glaucoma as well as patients with advanced glaucoma previously treated unsuccessfully with other surgical methods.
Endocyclophotocoagulation uses a microscopic camera which is placed inside the eye and allows visualization of the region that produces aqueous humor inside the eye. The laser is applied directly on this region and as a result the production of fluid inside the eye is reduced and subsequently intraocular pressure drops as well. It is suitable for patients who have been previously operated for cataract and they have intraocular lens inside the eye that we intend to operate with cyclophotophotocoagulation.
Trabeculectomy is a surgical procedure which creates a new pathway of drainage of fluid outside the eye, bypassing the trabecular meshwork which is not draining enough causing unacceptable levels of intraocular pressure.
In the anterior chamber of the eye there is an anatomic region called trabecular meshwork, through which the aqueous humor that is produced inside the eye drains out of the eye. When the aqueous humor is produced with a normal rate but is not properly drained outside the eye high intraocular pressure is noted.
Trabeculectomy creates an opening and a new path of communication between the anterior chamber and a new chamber called the bleb that is created outside the eye , just underneath the upper eyelid, in order for the fluid to drain.
Safe trabeculectomy is an improved trabeculectomy with impressive rates of success, which was developed in the
internationally renowned Moorfields Eye Hospital, in the United Kingdom, aiming at solving the basic postoperative problems: the abrupt drop of the pressure in the operated eye and the closure of the new opening that has been created for drainage due to the tendency of the organism to heal every trauma.
Specialized doctors at Moorfields found a solution to the first issue with the use of special releasable sutures that are placed during surgery. We have the potential to regulate the intraocular pressure postoperatively by removing these sutures if the pressure is above target avoiding at the same time very low pressures having placed enough tight sutures during the operation.
Intraocular pressure should not be too low after the surgery –a typical problem after traditional trabeculectomy operations – as the abrupt drop of the pressure can causes a shock to the eye and can be as damaging to the optic nerve as high pressure.
Thus, after surgery we are able to achieve pressure closer to the target pressure as determined before the operation in order to prevent further glaucomatous damage to the optic nerve.
During surgery and in the immediate postoperative period we also apply antimitotic agents in the newly formed drainage bleb underneath the upper eyelid. This will slow down the fibrotic process and prevents closure of the new draining pathway that was artificially created during the operation , therefore addressing the issue of scarring .
We aim is to maintain a steady satisfactory for the specific patient pressure and we keep him under close observation for three months after trabeculectomy, which is the normal recovery period. Thereafter, the intense monitoring stops and the patient can return to his everyday activities without the burden of frequent use of antiglaucoma medication and less chances of deterioration of his vision.
Through this process trabeculectomy becomes safer with high rates of success.
In the past few years, medical technology in the field of Ophthalmology has developed significantly and is offering Ophthalmologists a wide range of implants for treating all types of glaucoma, even the most difficult cases.
Amongst the most sophisticated implants are the glaucoma drainage devices, which are artificial plastic devices for drainage of the surplus of aqueous humor outside the eye, underneath the upper eyelid. With the help of these valves the dysfunctional trabecular meshwork is bypassed and the excessive aqueous humor finds a new exit in order to be drained smoothly outside the eye in a special bleb that is created under the upper eyelid. Some of them contain a sensitive inner valve that limits the flow of humor and prevents hypotony (very low pressure)
There are two basic types of valves:
- Ahmed and
- Baerveldt
According to the special characteristics of glaucoma that each patient has, the suitable type of valve is selected by the surgeon.
These valves are purposed for patients with uncontrolled glaucoma, with previous failed glaucoma operations but also for patients with progressive glaucoma for which classical trabeculectomy would have, for various reasons, low rates of success.
In the past few years, there has been a revolution in Glaucoma Surgery with the development of minimally invasive techniques. The benefit in these microsurgeries is increased patient safety. Since there is no surgical operation without risks, minimally invasive glaucoma surgery techniques offer improved safety and usually ensure a mild to moderate reduction of intraocular pressure.
These techniques either improve the drainage of aqueous humor by using titanium microcatheters (istent) at the level of trabecular meshwork or drain the humor outside the eyeball (e.g. XEN Gel Stent) or reduce the production of humor inside the eye (e.g. Endoscopic Cyclophotocoagulation).
Even though minimally invasive microsurgical techniques are not aiming to replace or eliminate the traditional surgical approach of glaucoma, they have reduced significantly the number of patients needing these more invasive surgical operations for controlling intraocular pressure.
Minimally Invasive Glaucoma Surgery techniques are constantly developing and reinforcing our weapons against the disease.
This constant technological development includes the use of new, innovative implants and sophisticated technology, some of which are available in Greece.
Dr. Koumoukeli, has trained extensively in the use of these sophisticated implants in Great Britain and she aims to become a leader in Greece in applying this technological revolution in glaucoma management.
Glaucoma and driving
Safe driving requires clear central eyesight and adequate peripheral eyesight. Glaucoma usually leads to loss of the peripheral visual field which affects significantly the patient’s ability to drive safely his car.
The effects of glaucoma in driving can be perceived in the form of peripheral cloudy vision and blind spots, poor night vision and reduced contrast sensitivity.
Glaucoma usually appears at the same age group as cataract and as a result difficulty in driving may be the consequence of either or both of these eye conditions.
According to studies, there are several problems associated with moderate loss of peripheral visual field secondary to glaucoma.
People that have lost some of their peripheral visual field due to glaucoma are at risk of not seeing a car or a pedestrian crossing the road or having a slower reaction due to reduced contrast sensitivity to any change in driving conditions.
All glaucoma patients must have regular follow-ups with their Ophthalmologist and check their visual field regularly in order to ensure that they are able to drive safely.